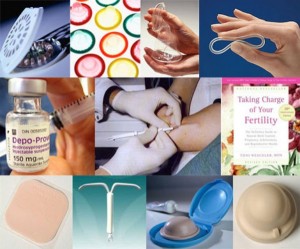
Modern Contraception Methods are presented and researched by Canadian Health and Care Mall online. We try to distinguish all the information exactly for you to make the choice easily.
Modern Birth Control Methods
Barrier Methods
Introduction
 Barrier methods are traditional and most ancient method of birth control. In the first half of the century various forms of barrier methods were virtually the only contraceptives. The advent of more effective contraception methods during the past 30 years has greatly reduced barrier methods popularity. However, complications that can arise when using a modern contraceptive methods, contraindications to the use, as well as a significant prevalence of diseases, sexually transmitted diseases, forced to improve barrier methods contraception methods.
Barrier methods are traditional and most ancient method of birth control. In the first half of the century various forms of barrier methods were virtually the only contraceptives. The advent of more effective contraception methods during the past 30 years has greatly reduced barrier methods popularity. However, complications that can arise when using a modern contraceptive methods, contraindications to the use, as well as a significant prevalence of diseases, sexually transmitted diseases, forced to improve barrier methods contraception methods.
The following types of barrier contraceptives exist:
- Women: non-drug barrier and medications;
- Men: barrier means.
Operation principles of barrier contraceptives are blocking sperm penetration in cervical mucus.
Advantages of barrier contraception methods include:
- they are used and perform only locally, without causing systemic changes;
- they have few side effects;
- they largely prevent some diseases, sexually transmitted diseases;
- they have virtually no contraindications for use;
- they do not require highly qualified medical staff assistance.
Indications for their use:
- contraindications to the use of oral contraceptives and IUDs (intrauterine devices);
- during lactation, as they have no effect on either the amount or breast milk quality;
- in the first cycle of oral contraceptives intake from the 5th day of your cycle, when natural ovarian activity is not yet fully suppressed;
- if necessary medication, can not be combined with oral contraceptives because it can reduce their efficiency;
- after spontaneous abortion until a period it is favorable time for new pregnancy;
- as a temporary means of production before male or female sterilization.
Disadvantages of barrier methods are as follows:
- They are less effective in comparison with the majority of oral contraceptives and intrauterine devices;
- In some patients it can not be used due to different manifestations of allergies to rubber latex or polyurethane; for their successful application it is required constant attention;
- Require the use of certain manipulation on genitals;
- Most of barrier contraceptive means are used during or immediately before intercourse.
Vaginal Diaphragm or Vaginal Pessary
It is suitable for contraception alone or in combination with spermicide. The diaphragm is a dome-shaped flexible rubber cap with a rim that is inserted into the vagina prior to intercourse so that rim is located in posterior vaginal fornix, anterior to pubic bone and dome to cover cervix.
The diaphragms are of different sizes from 50 to 150 mm. Nulliparous women generally are suitable vaginal aperture size of 60-65 mm, and giving birth women enjoy vaginal diaphragm size 70-75 mm. After birth, emaciation or size must be selected again.
Instructions for use: Woman when choosing diaphragm as a method of contraception, must be instructed by your doctor. Physician introduces it to pelvic and genital anatomy to female aperture arrangement represented in relation to cervix and uterus.
Installation procedure is as follows:
- Inspection of the woman and the selection of the diaphragm size and type.
- Introduction of the diaphragm: two fingers of right hand, squatting or lying on his back, inserted into vagina (left-handed woman spreads labia) in compressed form on the top and promotes it in the back wall of the vagina until it reaches the posterior vaginal fornix. Then, part of region, which was held last, pushed upwards until it touches the bottom edge of pubic bone.
- After diaphragm introduction a woman needs to palpation to check the location of diaphragm, covering cervix.
- Medical worker checks to determine whether woman has entered diaphragm correctly.
- Removing vaginal diaphragm should be carried out by pulling your index finger down the front edge. If there are any difficulties, woman should strain. After diaphragm removal it should be washed with soap and hot water, wipe off and put in 20 minutes 50-70 % of alcohol solution.
- Advantages of vaginal diaphragm are ease for use, multiple use opportunities, safety and significant degree of protection against sexually transmitted infections.
Contraindications
- endocervite;
- coleitis;
- cervical erosion;
- are allergic to rubber and spermicides;
- developmental abnormalities of genitals;
- ptosis of uterus and the vagina wall.
Side Effects
- possible infection of urinary tract as a result of diaphragm pressure on urethra;
- inflammation may occur at contact of diaphragm with vaginal walls.
Effectiveness
Pregnancy rates with the use of diaphragm coupled with spermicides is 2 pregnancies per year in 100 women using this method for a year regularly and correctly, and 10 pregnancies per year for every 100 women that have not undergone counseling.
Cervical Caps
Currently, there are three types of cervical caps that are made from latex rubber.
Cervical cap Prentifa – deep, soft rubber, with hard edges and notch to enhance suction. Its rim is pushed tight near the connection of cervix and vaginal vault. Prentifa cap sizes: 22, 25, 28, 31 mm (diameter of outer rim).
Cap Vimulya – a bell shape, more open end wider than body. Mounted directly on the cervix, but it closes open end and portion of vaginal vault. The cap is released in three sizes – diameter of 42, 48 and 52 mm.
Dumas cap has a flat configuration resembling a diaphragm but with the only difference that it is made of dense material and its rim has no spring. The cap is manufactured in 50 to 75 mm.
Fixed cap covers cervix, arches and upper part of vagina and held in place by the vaginal walls, but not at expense of adhesion to cervix.
Instructions for Use
The appropriate type and size of cervical cap are determined during the inspection of cervix’s shape and size. Introduction it through the vaginal opening is facilitated by the compression of edges, and placement of neck – by tilting cap into vagina. Before entering a cap on its inner surface spermicide preparation must be applied. After health worker found a woman cap, he must explain to her how to check means of proper installation and whether they closed cervix. Then she removes the cap and re-enters it, and health worker checks whether it is performing properly. It is not recommended that cap located in vagina for more than 4 hours.
Contraceptive Sponge
 In some countries – the US, Britain, the Netherlands – vaginal sponge has spread as an acceptable method of contraception.
In some countries – the US, Britain, the Netherlands – vaginal sponge has spread as an acceptable method of contraception.
Medical polyurethane sponge is soft flattened sphere with groove on one side, intended to be installed on cervix, and nylon loop on the other side, helping to extract this means. Sponge contains 1 mg as spermicide nonoxynol-9. The sponge performs as a barrier over cervix, carrier spermicide and ejaculate reservoir. The sponge can be administered one day prior to sexual intercourse and leave in vagina for 30 hours.
Condom
Condoms are the only contraceptive means used by men. A condom is a saccular formation of thick elastic rubber, about 1 mm in thickness, whereby it is possible to increase condom according to penile size. Condom length is 10 cm, width is 2.5 cm.
Application: Condom puts on the penis in state of erection, when balanus is not covered by foreskin.
Prevalence: The prevalence of this method is 20-30%.
Condoms Disadvantages
It is estimated that condoms “fail” in 10-30% of cases. Since negative effects lead even to the only “non-operation”, in general, effectiveness of such protection is unacceptable low.
There are several reasons for it: breakage or slippage during use, defective condoms that have been damaged or made with the factory defects (invisible to eye microscopic holes, sufficient for penetration of sperm and bacterial flora), cracked condoms due to improper storage conditions (kept in a hot or very cold place), and so on.
In addition, a condom, even completely high quality, virtually stops transmission of viral infections. Viruses, like bacteria and sperm are very small and are only visible in electron microscope. Electron microscopes, giving a high quality image of viruses show voids in the thin film of any condom rubber, that is through which viruses enter organism almost 50 times higher (!) than AIDS virus.
As an analogy, you can imagine that we throw a small stone in the volleyball net, and we hope that the stone will not fly through it. Of course, latex molecules can be “sewed” by chemical bonds stronger without these “big holes”, but then latex loses its elasticity – it becomes hard, brittle and unsuitable for condoms production (such rubber called vulcanite and is used in electrical engineering for insulators manufacture).
Along with AIDS virus is much more real and dangerous (many tens of thousands of times) the transfer of other intracellular infections – chlamydia, toxoplasmosis, herpes simplex virus, Epstein-Barr virus, hepatitis B and C, cytomegalovirus, enterovirus, human papillomavirus, and many others also sexually transmitted diseases which can easily penetrate through condoms.
The use of condoms inevitably leads to decrease in sexual sensation of partners; accurate putting on a condom is inconvenient procedure before sexual intercourse; may cause allergic to latex rubber or grease after condom application.
At sufficiently long intercourse condom slips almost always, but you do not feel it and observed it only after sexual intercourse completion, when sperm has been poured into vagina and sperm and infection transmission has already occurred.
When putting the condom at the end of sexual intercourse, it does not protect against diseases and does not provide sufficient protection against pregnancy. There is no guarantee that during process of sexual intercourse male urethral “lubrication” is not contained sperm.
Advantages of Condom are the following:
- condom is easy to use;
- the condom is applied immediately before sexual intercourse (but sexual intercourse should not be long-lasting);
- good-quality condoms (while maintaining in process of sexual intercourse of integrity) prevent pregnancy as well as bacterial infection diseases, sexually transmitted diseases, but in practice does not protect against viral (including HIV) infections.
Advances in contraception allowed to reduce the risk of unwanted pregnancy. At the same time in the last decade after the onset of AIDS, more and more attention is paid to the problem of sexually transmitted diseases (STDs), especially when it became clear that AIDS is not a “privilege” for specific populations, but manifestation of the very grave forms of immunopathology.
When there is a real danger of pregnancy, if during sexual contact ineffective contraception (vaginal douching or washing with a jet of water from the shower) is still applied or not applied, there are two exits – emergency contraception or, in the case of pregnancy, abortion.
Chemical Contraception
 The mechanism of spermicides action is to inactivate sperm and prevents its penetration into uterus. The main requirement for spermicide, is ability to destroy sperm for a few seconds. Spermicides are available in the form of creams, gels, foam aerosols, which poses suppositories and foaming tablets. Some women use for contraception after intercourse douching solutions having spermicidal action, acetic, lactic or boric acid, lemon juice. Given the evidence that 90 seconds after sexual intercourse in the fallopian tubes sperm is determined, douching with spermicidal preparation can not be considered a reliable method of contraception.
The mechanism of spermicides action is to inactivate sperm and prevents its penetration into uterus. The main requirement for spermicide, is ability to destroy sperm for a few seconds. Spermicides are available in the form of creams, gels, foam aerosols, which poses suppositories and foaming tablets. Some women use for contraception after intercourse douching solutions having spermicidal action, acetic, lactic or boric acid, lemon juice. Given the evidence that 90 seconds after sexual intercourse in the fallopian tubes sperm is determined, douching with spermicidal preparation can not be considered a reliable method of contraception.
Modern spermicides consist of spem-cells inhibiting substances and media. Both components play an equally important role in ensuring contraceptive effect. Carrier provides a dispersion of chemical substances in vagina, cervix enveloping and supporting it so that none of sperm could not avoid contact with spermicidal ingredient. The active ingredient in most modern spermicides are potent surfactants, destroying cell membrane of sperm. It is nonoxynol-9, menfegol, and benzylalkonium chloride. Product form spermicidal drug depends on its carrier.
Application: Spermicides can be used with condoms, diaphragms, caps and independently. Spermicides are introduced into upper part of vagina 10-15 minutes before sexual intercourse. For one sexual act, a single use of drug is required. Each time you have sex you need additional administration of spermicide.
Spermicides Advantages:
- ease of use;
- ensuring a certain degree of protection against certain diseases, sexually transmitted diseases;
- they are simple spare resources in the first cycle of oral contraceptive.
Disadvantages of this method is a limited period of effectiveness and need for some manipulation of genitals.
Efficiency: The frequency of spermicides isolated use failure varies from 3 to 5 pregnancies per 100 women per year when this method is used correctly. On average it is about 16 pregnancies per 100 women-years.
Biological Method
Introduction
Biological (rhythm or calendar) method is based on periodic abstinence from sexual activity in periovulation days. The biological method is also called the method of periodic abstinence, rhythm method of contraception, natural family planning method and method of determining fertility. According to the WHO definition, fertility control method is a method of planning or preventing pregnancy by determining the fertile days of menstrual cycle, during which the woman relies on periodic abstinence, or other methods of birth. Despite considerable progress of methodological options, value of functional diagnostics tests for determining functional state of reproductive system that are affordable and easy to follow, have not lost their relevance. At present, four methods of fertility control are used: calendar, or rhythm, temperature, Symptothermal method and cervical mucus method.
The Calendar (rhythm) Method
This method is based on the fact that ovulation has developed 14 days prior to the onset of menstruation (for a 28-day menstrual cycle), duration of sperm viability in women (approximately 8 days) and the egg after ovulation (usually 24 hours).
Instructions for use is as follows:
- using the calendar method of contraception you need to follow a menstrual calendar, noting duration of each menstrual cycle for 8 months;
- it should establish the shortest and longest menstrual cycles;
- using the method for fertility interval calculation is necessary to find the first “fertile day” (according to the shortest menstrual cycle) and the last “fertile day” (according to the longest menstrual cycle);
- then, given the duration of current menstrual cycle, determine range of fertility;
- during the same period it can be either completely abstention from sexual intercourse or you may use barrier methods and spermicides to prevent unwanted pregnancy.
The calendar method of contraception is not effective with irregular menstrual cycle. The effectiveness of calendar method is 14,4-47 pregnancies per 100 woman-years.
Temperature Method
This method is based on definition of recovery time of yellow basal body temperature by daily measurement. Considered fertile period of the menstrual cycle beginning as long as its basal temperature is raised for three consecutive days. Despite the fact that need for daily temperature measurement and prolonged abstinence period is limited the spread of this method, however its effectiveness is 0,3-6,6 per 100 women-years.
Cervical Technique
This method is based on the changing nature of cervical mucus during the menstrual cycle and is known as method of Natural Family Planning. After menstruation and prior to ovulation cervical mucus is absent or occurs in small amounts with a white or yellowish tinge. In pre-ovulatory days, mucus becomes more abundant, light and supple, mucus stretch between your thumb and forefinger reaches 8-10 cm. Ovulation occurs day after the disappearance of characteristic mucus (fertile period will continue further to 4 days after disappearance of light, flexible discharge). The effectiveness of cervical method ranged from 6 to 39.7 pregnancies per 100 woman-years.
Symptothermal Method
It is a method that combines elements of calendar, cervical and temperature methods, taking into account characteristics such as pain appearance in the abdomen and meager bleeding during ovulation. Efficiency of symptothermal method has shown the following indexes: if you have sex only after ovulation, pregnancy rate is 2 per 100 women-years, but if you have sex before and after ovulation – pregnancy rate increased to 12 pregnancies per 100 women-years.
Intrauterine Contraception
History of Intrauterine Contraception
 The history of intrauterine contraception begins with 1909, when German gynecologist Richter suggested that contraception one of method is that to introduce into uterus 2-3 silk thread, twisted into ring. In 1929, another German gynecologist Graofenberg altered this ring, entering into it silver or copper wire. However, construction was stiff, caused difficulties in introducing or removing, causing abdominal pain, bleeding, and therefore not widely used. It was only in 1960, when, thanks to the use of plastic Lippes Loop IUD type, intrauterine contraception has been applied widely and inert flexible plastic has been established in medical practice (IUD – intrauterine device).
The history of intrauterine contraception begins with 1909, when German gynecologist Richter suggested that contraception one of method is that to introduce into uterus 2-3 silk thread, twisted into ring. In 1929, another German gynecologist Graofenberg altered this ring, entering into it silver or copper wire. However, construction was stiff, caused difficulties in introducing or removing, causing abdominal pain, bleeding, and therefore not widely used. It was only in 1960, when, thanks to the use of plastic Lippes Loop IUD type, intrauterine contraception has been applied widely and inert flexible plastic has been established in medical practice (IUD – intrauterine device).
Hypothesis Related to IUD Mechanism
Today, there are several hypotheses about intrauterine contraceptive mechanism of action.
Hypothesis abortive IUD action. Under the influence of IUD endometrium trauma occurs with prostaglandins release, muscle tone of the uterus is increased, which leads to embryo expulsion at early stages of implantation.
Hypothesis of accelerated peristalsis. IUD enhances reduction of fallopian tubes and uterus so the fertilized egg enters the uterus prematurely. Trophoblast is still defective, endometrium is not prepared to accept a fertilized egg turning out to be impossible as a result of implantation.
Hypothesis of aseptic inflammation. IUD as a foreign body causes leukocyte infiltration of endometrium. Emerging endometrial inflammatory changes prevent implantation and further development of blastocyst.
Hypothesis of sperm toxic action. Leukocyte infiltration is accompanied by an increase in number of macrophages which carry phagocytosis of spermatozoa. Addition of copper and silver to the IUD increases sperm toxic effect.
The hypothesis of enzyme disturbances in endometrium. This theory is based on the fact that IUD enzymes cause changes in endometrium content that adversely affects implantation process.
Types of IUDs
There are now more than 50 kinds of IUDs of plastic and metal, which differ from each other in hardness, shape and size.
There are three generations of intrauterine devices.
- Inert IUDs. The first generation of IUDs is the so-called inert IUDs. The most widely used contraceptive was made of polyethylene in the form of the Latin letter S – Lippes loop. In most countries the use of inert IUDs is now prohibited, as it is seen in their application a lower efficiency and higher expulsion rates in comparison with using spirals of later generations.
- The copper-containing IUDs. They belong to the second generation. The basis for the creation of IUDs with copper were the experimental data showed that copper has a significant contraceptive effect in rabbits. The main advantage of copper IUDs compared with inert was a significant increase in efficiency, better portability, ease of administration and removal. The first copper-containing IUDs have been made in the design to include a copper wire of 0.2 mm diameter. Because copper is released quickly, it was recommended to change IUDs every 2-3 years.To increase the duration of IUD it is used techniques to slow down the fragmentation of copper: an increase in wire diameter, including a silver rod. It was created and evaluated many types of copper IUDs.
- Hormonal IUDs. They belong to the third generation of intrauterine device. A prerequisite for new type creation of IUD was desire to combine the advantages of two types of contraception – oral contraceptives and IUDs, reducing disadvantages of each. By this kind spirals are looked like T-shaped which is filled with hormone – progesterone or levonorgestrel. These spirals have a direct local effect on endometrium, fallopian tubes and cervical mucosa. The advantage of this spiral is to reduce hyperpolymenorrhea, reducing genitals’ inflammatory diseases frequency. The disadvantage is the increase in “inter-menstrual spotting.”
Contraindications to IUDs’ Use
Absolute contraindications:
- acute and subacute inflammation of genitals;
- confirmed or suspected pregnancy;
- confirmed or genital malignancy.
Relative contraindications:
- abnormal development of reproductive system;
- uterine fibroids;
- endometrial hyperplasia;
- hyperpolymenorrhea;
- anemia and other blood diseases.
IUDs’ Penetration Time
IUDs are usually administered on 4-6 day of menstrual cycle. During this period, cervical canal is slightly open, which facilitates procedures. Furthermore, at this time woman can be assured in pregnancy absence. If necessary, IUD can be introduced into other phases of menstrual cycle. The IUD may be administered immediately after abortion and postpartum. The main drawback of IUD at the time is a relatively high expulsion rates for the first few weeks. Therefore it is better to make IUD insertion after 6 weeks of postpartum.
IUD’s Application Methods
- The aseptic conditions cervix is exposed by mirrors with a disinfectant solution and capture upper lip by means of bullet forceps.
- Measure the length of uterine cavity via uterine sound.
- Using uterine sound IUD’s is administered into uterine cavity.
- Control study is made by means of uterine sound, making sure the correct position of IUD.
- Strands of IUD are clipped to length of 2-3 cm.
- Bullet forceps are removed and cervix is treated with disinfectant solution.
Methods of IUD’s Extracting
The cervix is exposed in mirrors. IUD’s having filaments usually removed by forceps. In the absence of threads with great care we can use royal crochet.
Follow-up after IUD insertion. The first medical examination is carried out after 3-5 days after administration, and then sexual activity is allowed without using any other birth control. Repeated inspections should be conducted preferably every 3 months.
Intrauterine Device Admissibility
Intrauterine contraceptives are an excellent reversible method of contraception.
Intrauterine Device has the following advantages:
- IUD’s use is not associated with an interference with woman’s normal life;
- After IUD insertion is usually needed only minimal medical care and supervision;
- IUDs are possible kind of contraception for older women, especially in cases where oral contraceptives are contraindicated;
- IUD can be used during breast-feeding;
- Possibility to use for a long time (5 to 10 years);
- An economic factor: the overall annual costs associated with the use of IUDs are relatively small for both women and for family planning programs.
IUDs’ efficiency: The contraceptive efficiency of IUDs is on average 91%, IUD with copper – 98%. For a more objective assessment of IUDs effectiveness is determined by Pearl Index, which is calculated by defining the number of pregnancies per 100 women using IUDs for 12 months. The statistical data is as follows: the number of pregnancies x 1200 / number of menstrual cycles. When using pregnancy rate was 5.3 / 100 woman-years. The introduction of the first copper-containing IUDs reduced pregnancy rate to less than 2/100 women-years, and the use of more modern copper IUDs resulted in lower pregnancy rates to the level of 0.4-0.5 / 100 woman-years.
In case of pregnancy with an IUD and woman’s desire to continue pregnancy if IUD threads it should be removed. In the absence of filaments it is required very careful monitoring of pregnancy. It should be noted that in literature there is no indication of an increase in malformations frequency or any damage to fetus if pregnancy is observed on background of IUDs. In women using IUDs, generative function is not impaired. Pregnancy occurs after IUDs’s extraction during the year in 90%.
Application Complications
Canadian Health and Care Mall points out that the early complications and side reactions that may occur after IUD insertion include:
- discomfort in the lower abdomen;
- back pain;
- cramping abdominal pain;
- bleeding.
Pain is usually held after taking analgesics, spotting can last up to 2-3 weeks.
Expulsion: In most cases expulsion occurs within the first few weeks after IUD insertion. Expulsion are more common in young, nulliparous women.
Bleeding: Violation of uterine bleeding nature – the most common complication of IUDs use.
There are three types of changes in bleeding nature:
- increase in menstrual blood;
- a longer period of menstruation;
- intermenstrual allocations.
Decrease of menstrual blood loss is possible by assigning prostanglandine – inhibitors.
Inflammatory disease: An important issue of the relationship between IUDs and inflammatory diseases of pelvic organs. Extensive studies in recent years show a low incidence of inflammatory diseases of pelvic organs with use of IUDs. The risk increases slightly in the first 20 days after administration. In the following period (up to 8 years), the incidence rate is maintained at a consistently low level. According to recent data, the incidence of inflammatory diseases of pelvic organs is 1.58 / 100 woman-years, when IUDs application is carried out. The risk of disease is higher in women under the age of 24 years and is closely correlated with sexual behavior. Active and promiscuous sexual life significantly increases the risk of these diseases appearance.
Uterine perforation is among the most rare (1: 5,000), but serious complications of intrauterine contraception.
There are three degrees of uterine perforation:
- the 1st degree – IUDs are partially located in the uterine muscle;
- 2nd degree – IUDs is entirely in uterine muscle;
- 3rd degree – the partial or total output of IUD into peritoneal cavity.
At the 1 st degree of perforation it is possible to remove the IUD vaginally. In the 2nd and 3rd degrees abdominal perforation shows path deletion.
In conclusion, it should be emphasized once again that IUDs is the best means of contraception for healthy nulliparous women with a regular partner, and not suffering from any inflammatory diseases of genitals.
Hormonal Contraception
Types of Hormonal Birth Control
 Hormonal contraception is based on the use of synthetic analogues of natural ovarian hormones and is highly effective in preventing pregnancy.
Hormonal contraception is based on the use of synthetic analogues of natural ovarian hormones and is highly effective in preventing pregnancy.
Depending on the composition and methods of hormonal contraceptives use are they divided into the following types:
Combined estrogen drugs is the most common oral contraceptives due to high reliability and reversibility of action, acceptable cost and good tolerability.
In turn, oral contraceptives (OCs) are divided into three main types:
- Monophasic, having a constant dose of estrogen (ethinyl estradiol) and progestogen;
- Biphasic, in which the first 10 tablets contain estrogen, and the remaining 11 tablets are combined, ie contain both estrogen and progestin components;
- Triphasic preparations contain stepwise increasing dose of progestogen and estrogen varying the dose with a maximum content in middle of menstrual cycle.
Mini-pill contains 300-500 mg gestagens per pill and does not limit significantly ovarian function. Acceptance begins with the 1st day of menstrual cycle and continue daily.
Postcoital preparations consist of large doses of progestin (0.75 mg levonorgestrel) or of large doses of estrogen (diethylstilbestrol, ethinyl estradiol). Estrogen dose is 2-5 mg, that 50 times higher than estrogen-gestagen combination preparations. These tablets are used for the first 24-28 hours after intercourse (in rare cases).
Long-acting formulations contain 150 mcg.
Slow-release drug contains 150 mcg depot medroxyprogesterone acetate or 200 mcg of NETA. Drug’s injection is made 1 time in 1-5 months.
Subcutaneous implants are silastic capsules that are administered subcutaneously in the shoulder region and emitted levonorgestrel daily, providing contraception for 5 years.
The vaginal progestin ring releasing is administered at 1 or 3 cycles.
Rogestasert is intrauterine device containing levonorgestrel in root, which throughout the year daily releases 20 micrograms of levonorgestrel.
Combined Oral Contraceptives
These drugs are the most common in the world form of hormonal contraception. Since the beginning of their use COCs have undergone significant changes in the dosage of steroids. The newest drugs containing 20 mcg of ethinyl estradiol.
Combined Oral Contraceptives
These drugs are the most common in the world form of hormonal contraception. Since the beginning of their use COCs have undergone significant changes in dosage of steroids. Doses of ethinyl estradiol and mestranol (estrogens used in COCs) have been significantly reduced over the past three decades, from 150 to 30 micrograms. The newest drugs contain 20 mcg of ethinyl estradiol. The dose of progestin component has also been reduced. Tablets produced today contain 0.4-1 mg norethisterone, 125 mg of levonorgestrel or even smaller doses of the most potent and selective progestin.
Changing type of progestogen to COC it is possible to distinguish three generations:
The first generation drugs are COC containing norethynodrel acetate.
Second generation drugs contain progestin and levonorgestrel. Its activity is 10 times higher as compared with norethynodrel.
The third generation, are COCs, containing desogestrel, norgestimate, gestodene included in Femoden drug.
These progestins used in micrograms, without causing disturbances in the metabolism of lipids, are of less androgenic activity, not increasing the risk of cardiovascular diseases.
Depending on estrogen and progestin dose components COCs may produce mainly estrogen, androgen or anabolic effects.
Mechanism of Oral Contraceptives Action
The mechanism of action is based on blockade of ovulation, implantation, change transport gametes and corpus luteum function caused by combined oral contraceptives.
Ovulation: The primary mechanism of ovulation suppression is provoked by gonadotropin-releasing hormone (GAD) by hypothalamus. Indicator of hormonal ovulation suppression are observed when the lack of estrogen peak, follicle-stimulating hormone and interstitial cell-stimulating hormone in the middle of menstrual cycle, inhibition of normal postovulatory increase in progesterone serum. During menstrual cycle, estrogen production in the ovaries remain low, corresponding to the early follicular phase level.
Cervical mucus: Thickening and induration of cervical mucus become evident after 48 h after progestins’ administration. Sperm’s mobility and ability to penetrate cervical mucus is disrupted due to its compression and condensation; cervical mucus becomes of reticulated structure and has a reduced crystallization.
Implantation: Implantation of developing blastocyst is observed in about 6 days after fertilization. To ensure the successful blastocyst implantation there is necessity to have sufficient maturity surface with adequate endometrial glands secretion and appropriate structure for endometrium’s invasion. Changes in levels and violations of the ratio of estrogen and progesterone are likely to disrupt the functional and morphological properties of endometrium. All this violates implantation process. Fertilized egg implantation varies under the influence of hormones on secretion and motility of fallopian tubes. These changes disrupt transport of sperm, egg or embryo development.
Oral Birth Control Efficacy and Acceptability
Oral birth control pills are the only means of preventing pregnancy with 100% efficiency. To distinguish theoretical efficiency, which involves this method’s use without error and pills omission and clinical effectiveness, which is calculated based on the number of pregnancies in real world, taking into account the errors, making by women.
The most objective indicator of the clinical effectiveness is considered to be Pearl Index, which reflects the rate of pregnancy in 100 women during the year. Pearl Index is determined the number of pregnancies per 100 women using a contraceptive method within 12 months, according to the following formula: the number of pregnancies x 1200 / the number of menstrual cycles. For oral contraceptives Pearl Index is 0.2-1.
So, birth control pills meet many requirements of modern contraception:
- High efficiency in preventing pregnancy;
- Ease for use (coitus-independent);
- Impact reversibility.
Principles of Oral Contraceptives Use
Despite the fact that modern contraceptives contain low doses of hormones and are well tolerated, they still are drugs whose use has various limitations and contraindications. The basic therapeutic principle is the need to assign each woman the lowest dose of steroids, which can ensure optimum reliability of contraception.
Absolutely healthy women are recommended contraceptive means with not more than 35 mcg of ethinyl estradiol and 150 mcg levonorgestrel or 1.5 mg of norethisterone.
The most important task of physician is to identify women for whom hormonal contraception is strictly contraindicated, necessitating a thorough history and careful examination of each patient.
Contraindications for Contraceptive Means Application
Absolute contraindications to use of the following diseases are OCs, which are present in patient at the moment, or there is their presence of history:
confirmed or suspected pregnancy;
- cardiovascular diseases;
- thromboembolism;
- varicose veins if there is history of thrombophlebitis;
- brain vessels Disorders;
- malignant genital tumors and mammary glands;
- liver disease;
- sickle cell anemia;
- severe forms of preeclampsia in history;
- diabetes;
- high blood pressure;
- gallbladder disease;
- smoking;
- lower stasis ulcer;
- long-term cast;
- prediabetes;
- severe headache;
- significant headache attacks;
- significant excess weight;
- age 40 years and above;
- epilepsy;
- hypercholesterolemia;
- Kidney disease.
System Changes when Taking Birth Control Pills In
Birth Control Pills intake may provoke adverse effects appearance on cardiovascular system; metabolic and biochemical processes; liver; some forms of cancer. It should be emphasized that all the above complications relating to taking pills containing estrogen and 50 mg progestogen high in the 1st and 2nd generation. It should be underlined negative effects do not occur when contraceptives are of lower doses of estrogen and progestin of 3rd generation. In addition, there are a number of risk factors contributing to the occurrence of complications during such pills application: smoking; obesity; age over 35 years; severe toxicosis in history.
The cardiovascular system: It is known that estrogens cause hypervolemia and has a stimulating effect on myocardium, which leads to a decrease in hemoglobin and blood-viscosity. Increase in circulating blood volume is determined because taking COs increases aldosterone production in adrenal cortex, thereby increasing sodium re-absorbation in renal tubules and osmotic pressure of blood plasma. Along with this, when receiving contraceptive means online increases systolic cardiac output.
Hypervolemia and activation of renin-angiotensin system COs contribute to arterial hypertension development, the incidence of which ranges from 2.5 to 6% of cases. The literature data on the incidence of myocardial infarction in women taking birth control pills is contradictory. It is believed that it is observed when taking contraceptive means increase in blood cholesterol, triglycerides, phospholipids and lipoproteins and contributed to development of myocardial infarction, especially if these changes are combined with other risk factors.
It should again be emphasized that changes in lipid metabolism and hypertension in women taking contraceptive means, are associated with a dose of estrogen component, as at lower doses of estrogen, these changes are reduced, while taking progestogen-only are not observed at all. If risk of myocardial infarction in non-smokers is not present while taking these pills, but frequency of heart attacks is increased by 2 times in case of taking birth control pills or smoking. With the combination of these factors, the risk of heart attack increases by 11.5 times.
The most serious complications when receiving contraception of oral type are related to thromboembolism. Estrogens increase the majority of indicators of blood coagulation, while anticoagulant factor – antithrombin III – is reduced. It trends towards increased platelet aggregation. The result may be thrombus. Oral contraceptives with estrogen content of more than 50 micrograms frequency increased lethal embolism by 4-8 times. Using medications of the latest generation, containing low doses of estrogen – 20-35 mg, only a few deaths from embolism are observed compared with not using contraceptives.
The risk of thromboembolism in women who smoke is increasing. Smoking increases the mortality from thromboembolism in women taking birth control pills, over age of 35 years – in 5 times and over 40 years – in 9 times. It should be noted that mortality from thromboembolism in smoking women is 2 times higher than that of non-smoking. The combination of several risk factors in women taking birth control pills, increasing the likelihood of thromboembolism in 5-10 times. In appointing such medications you should always remember that the risk of thromboembolism associated with oral contraception reception, is 5-10 times less than the risks associated with normal pregnancy and childbirth.
Carbohydrate metabolism: Estrogenic contraceptive means’ component violates glucose tolerance and leads to changes in carbon metabolism, characteristic of diabetes in 13-15% of women. Impaired glucose tolerance, which appears on a background of birth control pills reception, similar changes in carbohydrate metabolism, are observed in obesity, hypercorticoidism, in the III trimester of pregnancy. These changes are associated with impaired cortisol metabolism, since estrogen increases the number of circulating cortisol due to increased levels of transcortin. Increased cortisol levels associated with protein, cause a change in the content of enzymes in liver. At the same time there is an increase of free cortisol levels by 20-30%.
It should be noted that increase in incidence of diabetes in the group of women using contraceptive means, compared to control changes in carbohydrate metabolism in the body of healthy woman has transient character and disappears after canceling birth control pills. Moreover, these disturbances of carbohydrate metabolism are observed only when taking formulations containing high doses of steroids. Women with a previous glucose tolerance set must belong to the risk group and be under constant medical supervision. Oral contraceptives can be administered to young women with established diabetes in absence of other risk factors. Monopreparations containing only progestogen component affect carbohydrate metabolism to much lesser degree than combined. They are the drugs of choice of hormonal contraception in patients with diabetes.
Lipid metabolism: Oral contraceptives, estrogens have beneficial effects on fat metabolism by increasing the content of high density lipoproteins (HDL) and decreasing low-density lipoprotein (LDL). Progestin component of oral contraceptives have the opposite effect — it reduces the content of “good” HDL cholesterol and increase the concentration of “undesirable” LDL. Modern contraceptive means due to the change of quality and quantity of progestins (desogestrel, gestodene, norgestimate) do not have a pronounced effect on lipid metabolism. Birth Control Pills have effect on lipid metabolism being dependent not only on their chemical structure, but also on the initial level of lipid in each particular patient.
Oral contraceptives and liver disease: Steroids cause changes in liver function and degree of cholestasis. Canadian contraceptive means are contraindicated or should be used with a high degree of caution in the following conditions:
- for any active disease of liver with or without jaundice it;
- when infectious hepatitis is present intake of contraceptive remedies may be renewed in reduction of liver function;
- when selecting an alternative contraceptive is important to remember that pregnancy can be a greater burden on liver than contraception application;
- if there is a history of cholestatic jaundice during pregnancy or chronic idiopathic jaundice;
- in case of jaundice associated with oral contraceptives intake;
- with gallbladder diseases contraceptives do not contribute to formation of urine calculus, but can as well exacerbate existing disease.
Oral contraceptives and endocrine glands: Contraceptives have no significant effect on adrenal cortex and thyroid functioning. It is not identified a causal relationship between the use of combined oral and pituitary adenomas.
Oral contraceptives and fertility: After stopping ovulation contraceptive means recover quickly and more than 90% of women able to become pregnant for two years. The term “Post-pill” amenorrhoea is used to describe cases of secondary amenorrhea for more than 6 months after stopping contraceptive means application.
Amenorrhea lasting more than 6 months occurs in about 2% of women and especially typical for the early and late periods of reproductive fertility.
Oral contraceptives and pregnancy: Women who used birth control pills, no increased incidence of miscarriage, ectopic pregnancy, or violations of fetus are observed. In the rare cases when a woman accidentally tried contraception during early pregnancy, also are not revealed their damaging effect on fetus.
Oral contraceptives and age: The importance is the question of age at which a woman may start taking oral contraceptives for the prevention of unwanted pregnancies. Previously, there was a bias in relation to oral contraception appointment for adolescent girls. At present such ideas are rejected. In any case, use of pills is a better alternative to pregnancy and abortion especially in adolescence. It was proved that oral contraceptives do not affect weight gain and do not increase risk of amenorrhea.
The need for effective contraception is evident in the period preceding menopause. In cases when a woman and her partner are not acceptable other methods of contraception, when excluded the risk factors for cardiovascular and metabolic complications, such as hypertension, diabetes, obesity, hyperlipidemia, can be taken contraceptive means before menopause. A woman’s age is not as important in the absence of risk factors. Creating a modern oral contraceptives with low doses of hormones allows their use in women under 45 years of age or older. The drug of choice at this age may be drugs that contain only progestogen.
Oral contraceptives and lactation: Combined contraceptives undesirably affect the quantity and quality of milk, and can reduce the duration of lactation, so they should not be administered prior to breastfeeding termination. If a woman wants to use oral contraceptive means during lactation, only progestin contraceptives should be applied.
Canadian Birth Control Pills Effect Duration
With constant medical supervision, in case of contraindications absence women can continue taking birth control pills for many years. There is quite justifiable reasons for periodic abstinence from oral contraceptives.
Canadian Pharmacy Birth Control Pills Interaction with Other Drugs
In case of Canadian Pharmacy Birth Control appointment must consider possibility of drug interactions with a variety of drugs, which manifests itself in weakening of its contraceptive effect, in the case of simultaneous application.
These drugs include the following:
- Analgesics;
- Antibiotics and sulfonamides;
- Antiepileptic drugs;
- Sleeping pills and tranquilizers;
- Antipsychotics;
- Antidiabetic agents;
- Gipolepidemicheskie means;
- Cytostatics;
- Muscle relaxants.
Adverse Reactions and Complications
Adverse reactions and complications while taking contraceptives is mainly related to violation of estrogen-progesterone balance. They most often occur in the first 2 months of contraception reception (10-40%), and then is observed only 5-10% of women.
Adverse reactions when taking contraception due to excessive content of estrogen or progestin component:
- headache;
- weight gain;
- hypertension;
- fatigue;
- nausea, vomiting;
- depression;
- dizziness;
- decreased libido;
- irritability;
- acne;
- breast tenderness;
- baldness;
- thrombophlebitis;
- cholestatic jaundice;
- Leucorrhœa;
- headache between contraceptive means intake;
- chloasma;
- scanty menses;
- leg cramps;
- hot flashes;
- bloating;
- rash;
- vaginal dryness.
Adverse reactions while taking contraceptive means disadvantage caused hormones:
- Lack of estrogen: irritability; hot flashes; intermenstrual spotting in the early and mid-cycle; scanty menses; absence of menstrual reaction; decreased libido; reduction in size of mammary glands; dryness of vagina; headache; depression.
- Lack of progesterone: intermenstrual spotting at the end of menstrual cycle; heavy menstruation with clots; heavy menstruation with clots; menstrual – resembling delayed reaction after birth control pills.
Triphasic Contraceptive Means
At present, contraception choice is quite wide and, depending on the type and dose of the estrogen and progestin components of possibility of individual selection of drug have increased significantly. Singling out a three-phase oral contraception, it should be noted a significant reduction in dose of estrogen and progestin component
Triphasic contraceptive means consistently cause changes in level of estradiol and progesterone to mimic a much lower level of similar changes in normal menstrual cycle. Triphasic medications unlike other do not cause changes in glucose tolerance and lipid metabolism, and virtually no adverse effect on the hemostatic system that allows you to recommend them to women older than 35 years.
Mini-pills
One of promising directions of hormonal contraception development is to improve the mini-pill, or “pure” gestogens. These drugs do not contain estrogen microdoses consisting of synthetic progestogens (levonorgestrel, ethynodiol diacetate, norgestrel, etc.). “Microlut” (brand “Schering”) containing 300 mcg of levonorgestrel and is used not only as a contraceptive, but also as an effective therapeutic drug.
Mini-pill should be taken continuously, starting from the 1st day of menstrual cycle daily for 6-12 months. Usually, at the beginning of the use of mini-pills intermenstrual spotting is marked, the frequency of which is gradually reduced, and the 3rd month of admission completely stops. If intake of mini-pill provokes intermenstrual spotting, it is possible to recommend the appointment for 3-5 days, that is 1 pill that gives fast hemostatic effect. Since side effects of other mini-pill is not given, their use in clinical practice has broad prospects.
Action mechanism of contraceptive mini-pill is as follows:
- Changing the amount and quality of cervical mucus, increasing its viscosity;
- The penetrating ability of sperm decrease;
- The changes in the endometrium, excluding implantation;
- Inhibition of fallopian tubes motility.
Theoretically, efficiency of mini-pill is 0.3-4 pregnancies per 100 women-years, which is slightly higher than that of combined contraceptive means.
Mini-pill does not affect blood clotting, does not alter glucose tolerance. In contrast to the combined contraceptive means mini-pill does not cause changes in concentration of the main lipid metabolism indicators. Changes in liver while taking the mini-pill are negligible.
Based on the features of mini-pill, they can be recommended as a method of contraception in women with extragenital diseases (liver disease, hypertension, thrombosis states, obesity).
Mini-pill is particularly recommended in the following cases:
- women complaining of frequent headache, or increased blood pressure while using combined oral;
- lactation period 6-8 weeks after birth;
- diabetes;
- varicose veins;
- liver diseases;
- women older than 35 years.
Hormone Birth Control Pills
Postcoital Contraception
 The concept of hormonal postcoital contraception brings together different types of contraception, the use of which in the first 24 hours after intercourse prevents unwanted pregnancy. Postcoital contraception can not be recommended for continuous use, since each of methods is an extraordinary intervention in functional state of reproductive system with formation of subsequent ovarian dysfunction.
The concept of hormonal postcoital contraception brings together different types of contraception, the use of which in the first 24 hours after intercourse prevents unwanted pregnancy. Postcoital contraception can not be recommended for continuous use, since each of methods is an extraordinary intervention in functional state of reproductive system with formation of subsequent ovarian dysfunction.
Postcoital contraception include:
- Postinor containing one tablet of 0.75 mg progestogen levonorgestrel (taken in the first 24-48 hours 1 tablet 4 times every 12 hours).
- Oral contraceptives containing 50 mg of ethinyl estradiol (taken within 72 hours after intercourse to 2 tablets every 12 hours).
- Danazol (take 400 mg 3 times every 12 hours).
- IUD Cu-T 380 or multiload in the first 5 days after intercourse.
To the category of new contraceptives following types of contraception include:
- Depo-Provera, long-acting injectable medroxyprogesterone acetate;
- Norplant (levonorgestrel) in the form of an implant;
- Noristerat;
- Depot progesterone (norethisterone enanthate).
Depo-Provera is a sterile aqueous suspension of medroxyprogesterone acetate administered intramuscularly 1 time in 3 months.
Thus, contraception for a year provided only four injections. Pregnancy rate when using Depo-Provera is comparable to the described using oral contraceptives, ie, from 0.0 to 1.2 at 10 years of women when applied in a dose of 150 mg every 90 days.
Depo-Provera is particularly indicated for women in lactation period from 6 weeks after birth, at the age of late reproductive period in the absence of possibility to resort to surgical sterilization for women who are contraindicated for other methods of contraception in women with sickle cell disease, in which Canadian birth control means are contraindicated for the treatment of estrogen-dependent diseases.
Norplant – 6 is cylindrical capsules (containing levonorgestrel), which under local anesthesia is administered subcutaneously in forearm of left hand. The contraceptive effect is provided 5 years contraception. Efficiency is 0.5-1.5 pregnancies per 100 women-years for 1 year of Norplant use. Norplant may be introduced in the first days of the menstrual cycle, immediately after abortion, 6-8 weeks after birth. Chaotic spotting is observed in 2 out of 3 women during the first year of use.
Noristerat is a solution containing 200 mg norethisterone enanthate in 1 ml of oily solution. Intramuscular injection is carried out in the first 5 days of menstrual cycle, the next three injections should be carried out with an interval of 8 weeks. In the future, the interval shall be 12 weeks.
Noristerat application is contraindicated in diabetes, thrombosis, high blood pressure, acute and severe chronic liver disease with jaundice or without severe forms of diabetes, disorders of lipid metabolism, Dubin – Johnson syndrome, in case of herpes, transferred or concomitant liver tumors. When using Noristerat efficiency of 1.5 pregnancies per 100 women-years is recommended.
Voluntary Surgical Contraception (sterilization)
Introduction
Voluntary chemosterilization is the most effective and permanent method of protection for both men and women. At the same time, voluntary chemosterilization is safe and economical method of contraception. Improvement of anesthesia, surgical techniques and improved training of medical personnel are all contributed to improve the reliability of this contraception method for the past 10 years. Implementation of sterilization in the postpartum period in hospital does not affect the normal duration of menstruation.
The legal reasoning and health standards relating to use of voluntary chemosterilization, are varied. The first surgical sterilization has been applied to improve health, and later – to the wider social and contraceptive reasons. At the request of patients, surgical sterilization can be carried out under the following conditions:
the existence of family of at least two children;
Age of patient at least 35 years;
A written statement.
Medical indications are determined by the risk to health and life of women in subsequent pregnancies in the following conditions:
- Repeated cesarean section or uterine scar after conservative myomectomy;
- The presence of malignancy in the past in all locations;
- Diseases of the cardiovascular system;
- Respiratory diseases;
- Diseases of endocrine system;
- Mental diseases;
- Diseases of nervous system and sensory organs;
- Diseases of circulatory system;
- Diseases of digestive system;
- Disease of blood and blood formation;
- Diseases of urinary system;
- Diseases of musculoskeletal system;
- Congenital anomalies.
The decision to hold voluntary chemosterilization must be based on full awareness, careful consideration and the desire of the patient will no longer have children. Given the importance of volunteerism and the correct choice of contraceptive method, special attention should be given to consultation. The couple should realize the irreversibility of surgical sterilization method. When counseling patients doctor should guide by the following provisions.
 Advantages: one-time solution provides permanent, natural and most effective protection against pregnancy. Complications like any surgery, sterilization is linked with a number of potential complications (complications of anesthesia, inflammation, bleeding). Selection: along with sterilization patients should be advised reversible methods of contraception. Explained: the counselor should explain in detail and is available all the features and details of surgical sterilization, possible complications. It is necessary to emphasize the irreversibility of sterilization.
Advantages: one-time solution provides permanent, natural and most effective protection against pregnancy. Complications like any surgery, sterilization is linked with a number of potential complications (complications of anesthesia, inflammation, bleeding). Selection: along with sterilization patients should be advised reversible methods of contraception. Explained: the counselor should explain in detail and is available all the features and details of surgical sterilization, possible complications. It is necessary to emphasize the irreversibility of sterilization.
Patients should be informed that sterilization does not affect the health and sexual function.
Features of survey: patients should be given the opportunity to ask their questions to the choice of how contraceptive method was realized, and left no doubt. Patients should not feel any pressure from when choosing a method of contraception.
Voluntary Surgical Contraception for Women
Female sterilization is the surgical blockage of the Fallopian tubes to impede fusion of sperm and egg. This is accomplished by ligation, using special clips or rings, or electrocoagulation of fallopian tubes. Surgical sterilization is carried out in the postpartum period. In many countries, this method of birth control is performed immediately after birth (within 48 hours after birth). Thus, such operations in the United States comprise about 40% of sterilization. Feature of postpartum sterilization is determined by the fact that in the early postpartum period, the uterus and fallopian tubes are located high up in the abdomen. Minilaparotomy is performed through an incision of 1.5-3 cm in the suprapubic region.
Technique occlusion of fallopian tubes can be performed by the following methods:
Pomeroy Method – loop of fallopian tube is ligated catgut in its middle part, and then excised.
Pritchard Method (Parkland) lies in the mesentery excision of each fallopian tube in the avascular portion ligation pipe in two places, and excision of segment located between them.
Filshi Clip is applied to fallopian tubes at a distance of 1-2 cm from the uterus. After birth, the clamps applied slowly (to evacuate edema fluid from both tubes).
Electrocoagulation for postpartum sterilization is not recommended, because this method is used in laparoscopy. However, postpartum laparoscopy is rarely used.
Excision of uterus fallopian tube angle with its resection or removal. To reduce risk of ascending infection improves access for sterilization, fallopian tubes should be done 48 hours after birth. If sterilization is performed 3-7 days after delivery in the postoperative period, it is necessary to prescribe antibiotics. If sterilization is not made within 7 days of postnatal period, it is recommended to resort to sterilization after 4-6 weeks after birth. Voluntary Surgical Sterilization is often performed during cesarean section.
This method of sterilization should be selected by operating doctor. Before surgical sterilization of women is necessary to conduct a survey, which includes the following measures: clinical blood and urine analysis; blood chemistry; blood type, Rh factor, Wasserman and HIV; coagulation; study of vaginal content; ECG and chest X-ray; inspection of therapist.
Long-term effects and complications of sterilization reduced to a possible ectopic pregnancy, the onset of which can be attributed to the following factors: a) the development of utero-peritoneal fistula after sterilization by electrocoagulation; b) inadequate occlusion or recanalization of fallopian tubes. The effectiveness of the method is very high. The indicator “of contraceptive failure” is 0,0-0,8%.
Voluntary Surgical Sterilization for Men
Male sterilization, or vasectomy, is applied to block vas deferens to prevent sperm terrain. Vasectomy is a simple, inexpensive and reliable method of male contraception.
After consulting the patient and registration of legal documents, you must carefully collect anamnesis, find a history of bleeding, allergic reactions, diseases of cardiovascular system, urinary tract infections, diabetes, anemia and diseases, sexually transmitted diseases. At objective research it is determined pulse and blood pressure, skin and subcutaneous fat layer, perineum, presence of scrotum inflammation, varicocele, cryptorchidism.
Vasectomy Technique
First option. Vas deferens are located on both sides of scrotum, and fixed operating portion infiltrate 1% solution of novocaine. Over vas deferens is cut skin and muscle layer, insulated duct ligated and cross. Each segment can be cauterized or electrocoagulated. For greater reliability it is possible to remove a segment of vas deferens.
The second option. Vas deferens cross without dressings (the so-called open-end vasectomy of vas deferens) and is subjected to cautery or electrocoagulate to a depth of 1.5 cm. Then the fascial layer is applied to close the crossed ends.
Third option. “Droplet-free vasectomy” is that for vas deferens release it is applied puncture, and not cut. After a local anesthetic specially designed ring-shaped clamp is applied to vas deferens, without opening layer. Then dissecting clamp with the sharp end of small skin incision is performed and wall vas deferens, the duct is isolated and conducted its occlusion.
The indicator “failure” in male sterilization method is 0.1 to 0.5% in the first year. It is associated with vas deferens recanalization or unidentified congenital anomaly in the form of duplication ductus deferens.
Principles of Contraception Method Selection in Women with Extragenital Pathology
Birth control method selection in women with various extragenital diseases should be carried out according to contraindications those presented in the previous sections, a thorough history analysis of disease and individual characteristics of woman. The most common among extragenital diseases are diseases of cardiovascular system. In severe forms of heart diseases, coronary artery disease, acute thrombophlebitis, thromboembolic conditions, arterial hypertension of I and II degree it is recommended to give preference to IUDs, and chemical barrier methods of contraception, physiological method of hormonal contraceptives – mini-pills. In the most severe manifestations of cardiovascular disease – surgical sterilization is the most preferable.
Given peculiarity of estrogen it may cause hypervolemia stimulating myocardium, increasing systolic and cardiac minute output, in case of cardiovascular diseases COC’s use is contraindicated. At varicose veins but thrombophlebitis absence during the inspection and in history permissible use of estrogen-progestin Canadian birth control pills with low estrogen may be taken but under careful supervision of blood coagulation indicators state. Chronic, often relapsing inflammatory disease of respiratory system (bronchial obstructive disease, chronic pneumonia, etc.) any contraceptive method is not a contraindication.
In diseases of digestive organs (liver, cirrhosis, gastritis, cholecystitis, liver tumors, chronic gastritis) excludes choice of hormonal contraception. It is recommended to use IUDs, barrier and chemical methods, physiologic method. Contraception for chronic recurrent diseases of kidneys is determined by frequency of exacerbations.
During prolonged remission it is possible to use combined birth control pills with low estrogen level, IUDs and barrier chemical methods, physiologic sterilization. In diseases of nervous system (loss of brain vessels, epilepsy, migraine) and psychiatric diseases involving depression, hormonal contraception is contraindicated, but may be used IUDs, barrier and chemical contraception, physiological method.



